Consumers want to eat their way to better health. How can health and business leaders help?
A Deloitte survey finds that most US consumers want to use food to help manage their health, creating opportunities for health and business leaders
Ryder Riess
Kyle Vahle
Leala Shah Crawford
Dr. Jay Bhatt
Leslie Korenda
Wendy Gerhardt
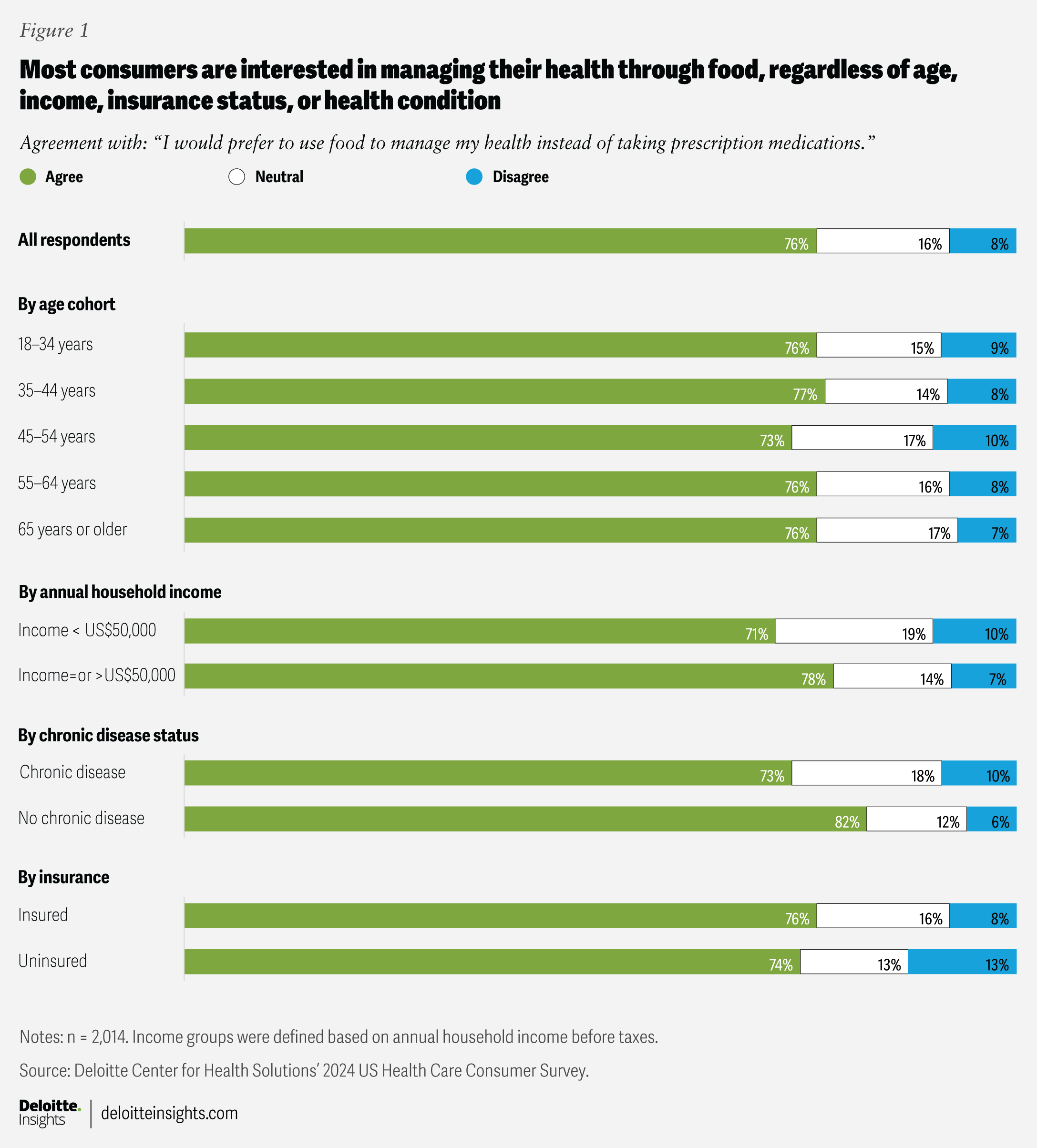
There’s a desire among US consumers to use food as a means of managing their health, based on findings from a Deloitte Center for Health Solutions survey. The survey reveals that 76% of Americans would prefer to use food over prescription medications to support their health, regardless of age, household income, insurance status, or health condition. While medications remain essential and valuable, nutrition is increasingly being recognized as a vital part of overall health management. Some patients with chronic illnesses are benefiting from food prescriptions, meal planning, and other nutrition-focused services as part of their care.1
Despite recognizing the link between nutrition and well-being, many consumers face obstacles to eating healthy—such as limited access to nutritious foods, high costs, and uncertainty about which options are best.2 Even when healthier options are available, convenience and ingrained habits can sometimes lead people to default to less healthy choices.3
There are opportunities for health care organizations, employers, grocers, technology companies, and other stakeholders to help consumers address these challenges. By making nutritious options more accessible and easier for consumers to understand, these groups can help address consumer challenges and positively influence health outcomes. Supporting healthy eating can help reduce chronic disease risk, improve well-being, and advance business goals.
To better understand consumers’ health experiences—and their attitudes toward nutrition and its impact on health—the Deloitte US Center for Health Solutions conducted a nationally representative survey of 2,014 US adults in July 2024 (see methodology). The 2024 US Health Care Consumer survey found that a majority of consumers recognize the effect food can have on their health, independent of their age, household income, insurance coverage, or whether they have a chronic condition (figure 1). The notion that “food is health” can present opportunities for stakeholders to promote healthy options for consumers. However, this task is likely to be complex and challenging and may require collaboration among various parties.
Consumers recognize the powerful effect of healthy food, but may face challenges
The daily food choices consumers make can influence their long-term health and risk of developing a chronic illness.4 Among the 76% of survey respondents who prefer to use food over prescription medications to manage their health, 45% have at least one chronic condition . Of those respondents with a chronic condition, 73% expressed interest in using food to manage their health as much as possible (figure 1). Among respondents without a chronic illness, 82% preferred to use food to manage their health. This strong preference across both groups indicates a potential opportunity for dietary interventions. However, for many, prescription medications remain an important and necessary tool, highlighting the complementary roles of nutrition and medical care.
While a majority of surveyed consumers expressed interest in using food to help manage their health, maintaining a healthy diet can be challenging. About 1 in 7 US households lacks access to affordable and nutritious food.5 Nutrition-related illnesses such as obesity, diabetes, and cardiovascular disease are most prevalent in rural, inner-city, and lower-income areas, due in part to limited access to affordable or accessible healthy food.6 Recent findings from Pew Research Center indicate that about 70% of Americans say the rising cost of healthy food has made it more difficult to maintain a healthy diet. This sentiment is more common among lower-income individuals, with 77% expressing this concern compared to 54% of higher-income individuals.7
In addition to broader economic challenges, healthy foods tend to be more expensive than unhealthy options because of transportation costs, limited shelf life, and supply chain complexities.8 For instance, fish, meat, and certain types of fresh produce require refrigeration and frequent restocking, unlike more processed, shelf-stable options.
Moreover, information about the nutritional value of food—from product packaging, marketing, and nutrition labels to news reports and social media—can seem confusing, contradictory, or unreliable.9 Guidance on which foods are healthy—such as those labeled organic or promoted as low in carbohydrates, fats, or calories—can be conflicting.10 For example, a 2022 Deloitte survey found that 62% of consumers encounter conflicting information and may be confused about the healthfulness of specific foods. Moreover, 40% of those survey respondents indicated they do not clearly understand which fresh foods can improve health.11 Other factors, such as social influences,12 busy lifestyles,13 and lack of support,14 can also make it difficult for some consumers to transition to a healthier diet.
Proper nutrition is important for overall health and well-being
Nutrition can help prevent, manage, and treat certain health conditions.15 In practice, this may involve medically tailored meals, nutrition counseling, or food prescriptions for people with chronic diseases. These approaches are meant to complement—not replace—medical treatments, supporting better health outcomes through a holistic approach.
A healthy diet typically includes nutrient-rich foods like fruits, vegetables, whole grains, and lean proteins, according to the US Food and Drug Administration.16 It should also limit saturated fat, sodium, and added sugars.17 However, what constitutes a healthy diet can vary by individual, influenced by factors including food allergies, health status, chronic illnesses, genetics, and cultural influences.18 For this research, we did not define “healthy,” allowing survey participants to respond based on their understanding.
As consumers begin to recognize the connection between their food choices and long-term health—and given the challenges of making healthy food choices—many seek guidance and advice from trusted sources. Trust is a cornerstone of effective health care and can influence consumer behavior. According to the survey results, 69% of respondents reported having “high trust” in physicians for reliable information about healthy foods. Another 61% expressed high trust in nutritionists, and 42% reported high trust in pharmacists (figure 2).
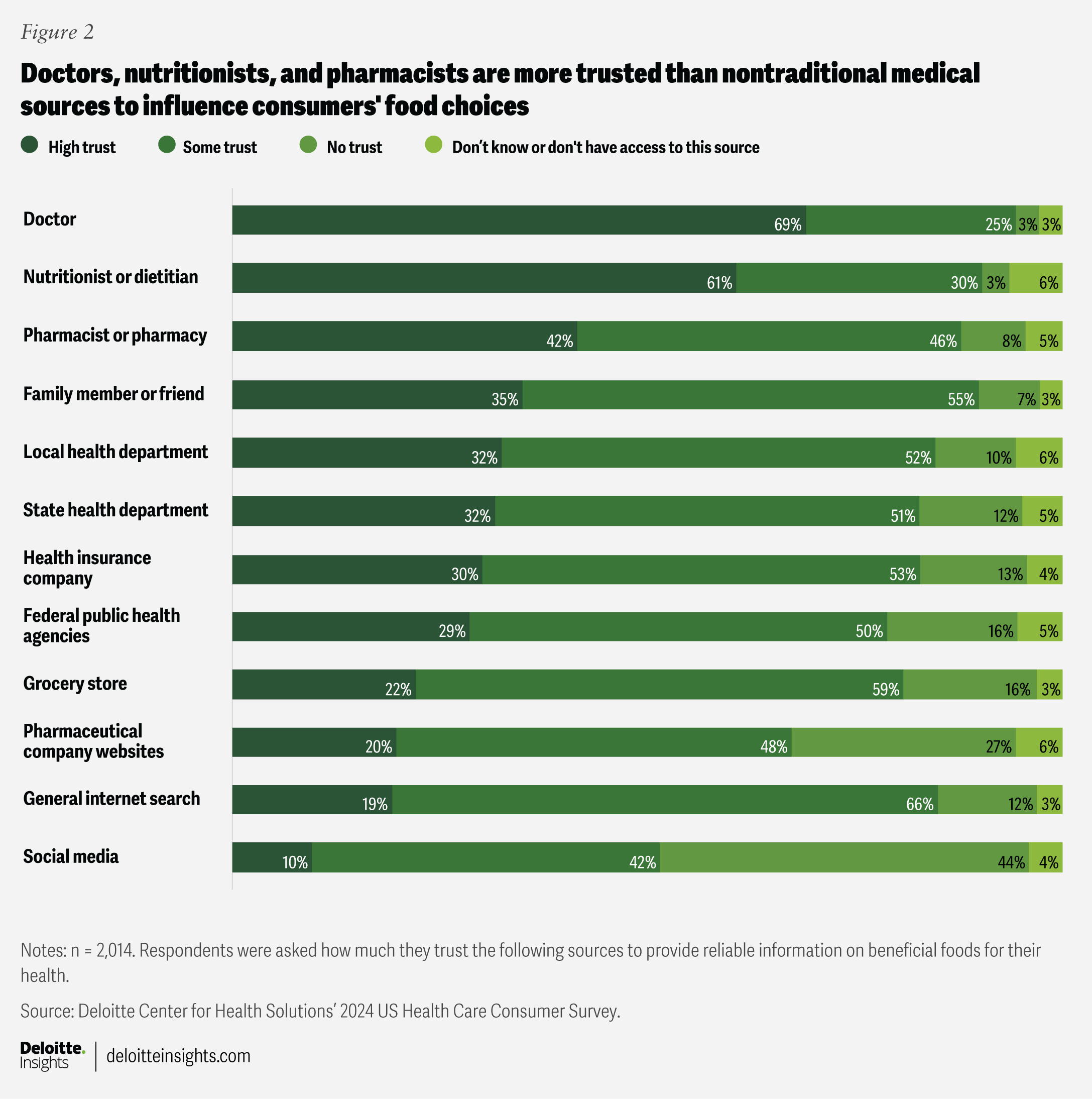
Physicians, nutritionists or dietitians, and pharmacists are often viewed as credible sources of health information and are considered more reliable than social media or other nontraditional medical sources (figure 2). However, physicians and pharmacists often lack the time and training to educate patients about healthy eating habits.19 A 2023 survey conducted by the University of Louisville found that 58% of US medical students received no formal training in nutrition.20 Additionally, only about 20% of medical schools in the United States require a dedicated nutrition course.21
Opportunities for stakeholders to improve health and margins
Using healthy foods to treat, manage, or prevent illnesses presents a potentially transformative opportunity to reduce the prevalence of some diseases, improve overall health outcomes, and lower health care costs. Seven of the 10 leading causes of death in the United States are directly affected by diet,22 with the cost to treat these illnesses exceeding US$400 billion annually.23 Adopting healthier diets could help reduce the prevalence and incidence of diet-related diseases and improve the overall health of Americans. This would likely translate to fewer hospital visits, reduced need for medications, and lower long-term care costs.24
Ensuring that healthy food is accessible, affordable, and tailored to individuals involves a collective effort and a multifaceted approach. Health care organizations, grocery and pharmacy retailers, and technology developers all have opportunities to help consumers make better dietary choices. While their efforts may not always result in immediate growth and improved margins, the overall business value tends to lie in improved health, which can have positive downstream impacts on businesses. For example, grocers could see increased sales, while health plans and employers could benefit from reduced medical costs. Additionally, stakeholders may experience improved workforce productivity through healthy food initiatives focused on employees. Improved health outcomes for patients, members, and employees—as well as enhanced community health—are likely not only goals for health systems but also part of the brand and marketing strategy for many health plans and grocers. Here are a few considerations for stakeholders:
Health plans
By enabling access to healthy food and integrating with programs that improve access to preventive services and early diagnostics, health plans have an opportunity to improve both the cost-effectiveness of care and health outcomes.25 Creating offerings that align with consumer preferences and are tailored to individuals can also help health plans improve member experience and satisfaction. Expanding nutrition-related services may be important for health plans, especially when demographics and competition can make growth challenging. Health plans should consider the following strategies:
- Enhance food-related offerings and financial support for all members: This could involve extending programs or payment mechanisms for food-related services—initially designed for specific members—to all interested members. Such services might include nutrition counseling, healthy meal plans, prepared meal-delivery services for patients, and weight management programs. For example, Kaiser Permanente provides a meal service for Medicare beneficiaries, delivering nutritionally complete, dietitian-designed meals to a member’s home or skilled nursing facility after hospital discharge.26
Blue Cross of North Carolina launched a program in 2021 for members with type 2 diabetes who are considered at high risk for food insecurity. Through the program, members receive two boxes of healthy foods each month and have access to nutrition counseling.27 Full participation in the program was associated with a reduction of US$139 per member per month in total medical costs and an increase of US$8 per member per month in pharmacy costs, suggesting greater medication adherence.28
Offering similar services to members who do not have chronic conditions or are not recovering from a hospital stay could help prevent future health issues and improve member engagement.
- Align with local grocers and social entrepreneurs using digital tools for consumer engagement: Health plans that offer food benefits might consider working with local grocers and food distributors to connect healthy food subsidies with approved grocery items. This collaboration could benefit consumers by improving access to healthy food and other stakeholders by increasing member satisfaction for health plans and generating increased revenue streams for retailers and distributors. Such alliances could also help ensure that consumers understand how to use their subsidies to purchase healthy food.
Health plans may also consider collaborating with social entrepreneurs who use digital tools to improve access to healthy food. For example, Fresh Connect enables health care organizations to prescribe and cover the cost of healthy food using prepaid credit cards. Its technology platform uses data analytics to provide tools and prompts that educate and support healthy food choices.29 Greens Health offers an AI-powered platform for personalized diabetes management, integrating meal planning, remote glucose monitoring, and social determinants of health screenings.30
Collaborating with grocers and social entrepreneurs could also provide health plans with valuable insight into the types of food their members purchase. This data could be used to influence future food purchases through real-time targeted nudges and interventions aimed at specific members, such as those with chronic health conditions. For example, a health plan might send reminders to members with diabetes or those at risk to get their A1c levels checked at the grocery store’s pharmacy. Additionally, the health plan could send educational prompts to all members about which healthy foods are in season, available, or on sale at their local grocery store. However, implementing this strategy will involve health plans ensuring that members’ shopping history and health data are protected from a privacy and confidentiality perspective.
Health systems and clinicians
Focusing on healthy food can yield direct financial benefits for health systems that generate revenue through value-based and risk-based contracts. However, it may represent an additional expense under a traditional fee-for-service model. Beyond the potential financial benefits, there may also be indirect benefits. Addressing this consumer need can help provider organizations boost consumer satisfaction, loyalty, trust, engagement, and retention, potentially leading to downstream revenue opportunities. Integrating healthy food programs with efforts to improve access to preventive services and early detection could also have a significant impact on health outcomes. Providers may also benefit from improved employee health and productivity.31 Further, this approach can bolster community health impact statements by providing specific examples of how health systems are improving access to, affordability of, and understanding of healthy food in the community. Health systems and clinicians should consider the following strategies:
- Equip clinicians with information about healthy food and nutrition: Doctors and pharmacists are among the most trusted sources of information on making healthy food choices (figure 2). Health systems can offer continuing education and other reliable resources on nutrition to their employed and affiliated doctors, pharmacists, and other clinicians. This can help ensure they are prepared to engage with and guide patients toward healthy food decisions. Health systems might also consider increasing the number of dietitians and nutritionists on staff and placing these professionals at various locations within the community.
- Collaborate with other stakeholders to provide trustworthy, reliable nutrition information and to improve access to healthy food: If unable to offer nutritional guidance themselves, health systems might direct consumers to certified nutritionists in the community, such as those available at community health centers or dietitians working within pharmacies or retail stores. Health systems can also work with technology organizations to provide reliable information. One example of such collaboration is Google’s partnership with Tufts University to explore technology solutions that help improve the quality of nutrition information.32
Health systems can also collaborate with stakeholders like social entrepreneurs to improve access to healthy food. Lemontree uses an SMS helpline to connect users with nearby free food resources. This solution is powered by a comprehensive data set of food resources, supported by real-time data from user feedback.33
- Serve healthy foods in care settings: Health systems could consider replacing unhealthy food options on their campuses with healthier meal choices for patients, caregivers, and employees. They might also implement and expand “food pharmacies” as an additional service. These food pharmacies, typically located on hospital campuses, provide free or subsidized healthy foods to patients with a doctor’s prescription. Health systems could expand this concept by offering such services at each of their community locations, in collaboration with local community health clinics, and as part of mobile clinics.
For example, NYC Health + Hospitals, which operates more than 70 health care facilities throughout New York City, has begun offering free boxes of fresh produce to patients who are enrolled in its Lifestyle Medicine Program. Through this program, patients work with dietitians to learn how to incorporate fruits and vegetables into their diets. Adults living with prediabetes, type 2 diabetes, high blood pressure, heart disease, or health concerns related to excess weight are eligible to enroll.34 Sodexo, a food service provider, plans to expand its plant-based meals program to all of its 400 US hospital sites. The company reports serving 290,000 meals each day in hospitals.35
- Expand food-related services to reach everyone: Provider organizations should consider enhancing their existing food-related services, such as nutrition counseling, healthy meal plans, online and on-call meal delivery services, and weight management programs. For example, Instacart and Mount Sinai Solutions partnered to offer US$110 grocery stipends to post-operative and postpartum patients. This arrangement provides access to fresh groceries via a tailored virtual storefront, supporting recovery and better patient outcomes.36 While the program specifically targets patients with chronic diseases, it could be expanded to help prevent or address health issues among other patients.
Food-related services should also be designed to encourage adherence. Rather than urging patients to eliminate familiar foods from their diet, nutritionists could explain how to modify meals to create healthier options that align with dietary recommendations.37 By understanding and incorporating cultural food preferences, dietitians, clinicians, and health systems can promote better adherence to dietary recommendations and improve overall health. People are more inclined to make changes that respect their culture, traditions, and preferences.38
Retailers and grocers
Retailers and grocers have an opportunity to support and benefit from consumers’ preference for healthy food choices. By doing so, they can increase revenue, sales, build consumer loyalty, and compete on factors beyond price. While healthy food is a priority for many consumers, so is convenience.39 According to a 2024 Deloitte survey, 52% of consumers value convenience more now than they did in the past. A 2023 Deloitte survey of 100 grocery store executives revealed that 2 in 3 executives see a connection between increased interest in healthy foods and higher sales.40 Retailers and grocers should consider the following strategies:
- Improve access and convenience to healthy food: Grocers might be able to attract more shoppers by offering a variety of curated, health-conscious food options. They should also consider clearly identifying and labeling items that are healthy and potentially eligible for financial support. Programs could involve input from certified nutritionists and medical professionals or include tailoring food selections to meet the specific health needs of different groups—such as individuals with diabetes or heart disease—with clear labeling to indicate suitability for those conditions. Grocers can also make healthy food more convenient by providing options like pre-cut produce or grab-and-go meals, making them easier to prepare, consume, and clean up.
Grocers might also consider working with other stakeholders to create healthy food delivery programs, in-store healthy food labeling, food stipend programs, and meal-planning initiatives. For example, the ¡Más Fresco! More Fresh program is a partnership between Northgate González Market, UC San Diego Health, and the US Department of Agriculture.41 This initiative provides rebate dollars to low-income individuals in California when they purchase fresh, frozen, dried, or canned fruits and vegetables. Such collaborations could help retailers expand their customer base and increase revenue. Additionally, focusing on community health could lead to positive press, an enhanced brand image, and increased customer loyalty.42
- Use technology to enhance the shopping experience: Retailers should explore how technology can be used to promote healthy food choices. For instance, tech-enabled smart shopping carts could suggest healthy recipes or offer healthier alternatives to items placed in the cart. Grocers could also update their store apps to highlight healthy food options. By adopting these strategies, retailers could improve public health, drive business growth, and strengthen their competitive edge. Artificial intelligence tools could provide shoppers with personalized information and help them quickly locate healthy foods in the store.
- Capitalize on loyalty and reward programs: Grocers could incentivize consumers to purchase healthy foods by offering rewards, potentially linking these benefits to shared rewards with other stakeholders.
- Integrate trusted staff into healthy food programs: Nutritionists and pharmacists, who are often part of grocery store staff, are among the most trusted sources for healthy food information, according to the 2024 US Health Care Consumer Survey. Grocers could leverage these professionals to provide individual consultations and make them available in the healthy food sections of the store to answer customer questions.
Employers
Some employers have an opportunity to provide healthy food options to their employees. Such initiatives could improve workforce health, potentially increasing productivity and reducing the company’s health care costs, ultimately benefiting its bottom line. According to Deloitte research, employers can play an important role in helping Americans live longer and healthier lives. Employers should consider the following strategies:
- Help employees understand the connection between food and health: The Health Action Council (HAC)—a not-for-profit purchasing coalition comprising 230 self-insured mid-sized and large employers—is working to improve the health of employees and their families. A recent HAC study estimated that health care costs for workers with obesity were double those of workers without the condition. The study also found that children of parents with obesity tend to have higher medical costs than other children.43 To address these issues, the HAC encourages its member companies to educate workers about the role nutrition plays in health and to replace unhealthy breakroom and cafeteria foods with healthier options.
- Improve access to healthy foods: Employers might consider providing healthy snacks in the workplace or offering wellness stipends for food purchases. These initiatives can enhance employee satisfaction and boost productivity.44 Additionally, there may be opportunities to offer subsidies for medically tailored meals.45
- Collaborate with other stakeholders on healthy food offerings and services: Employers could work with their health plans to include food-related offerings in employee benefit packages. They might also collaborate with local grocers to deliver healthy food to the workplace or employees’ homes. Additionally, employers could offer access to nutritionist services at the workplace. However, when implementing these strategies, employers should ensure that health data is protected from a privacy and confidentiality perspective and that programs are designed to empower employees rather than track individual health.
Stakeholders should proactively consider how to measure the impact of these programs and assess their effectiveness. Developing scorecards that track and evaluate efforts can help ensure alignment with organizational goals. It is useful to tie these measurements to a broad range of business metrics, including financial performance, health outcomes, disparities, and consumer experience, to fully understand the impact. For collaborative programs, each participating organization may need to focus on sharing timely and accurate data with other stakeholders to evaluate the collaboration’s impact. Measuring consumer experience is particularly important for gathering feedback on changes in shopping and eating behaviors, as well as understanding participants’ satisfaction with the program.46
Collaborative efforts could promote healthier eating
Health systems, clinicians, employers, health plans, grocers, and retailers can all play a role in getting healthy foods into the hands of consumers. Integrating healthier food choices into consumers’ daily lives can help enhance public health, reduce medical expenses for health plans and employers, and create new revenue streams for retailers. This approach could also improve consumer engagement and loyalty for all stakeholders. Synergistic relationships between health plans, health systems, employers, and grocery retailers can help consumers understand the connection between healthy foods and well-being. Innovative strategies like food prescriptions, personalized nutrition plans, and subsidized healthy grocery options have the potential to revolutionize how health and wellness are perceived and managed.
When consumers focus on the link between nutrition and well-being, organizations that provide health care or sell food can play a bigger role in encouraging healthy eating habits and, as a result, help people become healthier. By investing in consumer education, accessible food options, and financial-support mechanisms, healthy eating could become more prevalent. This approach aligns with broader societal shifts toward preventive care and personalized health management,47 potentially improving individual health outcomes and maximizing economic benefits through reduced health care costs.
Methodology
Since 2008, the Deloitte Center for Health Solutions has conducted surveys of US adults to understand their experiences and attitudes related to health, health insurance, health care, and their views on the health system. This is the twelfth iteration of the survey. The survey was conducted in July 2024 and included a sample of 2,014 respondents aged 18 and over. The sample was representative of the US Census population in terms of demographics and health insurance coverage.