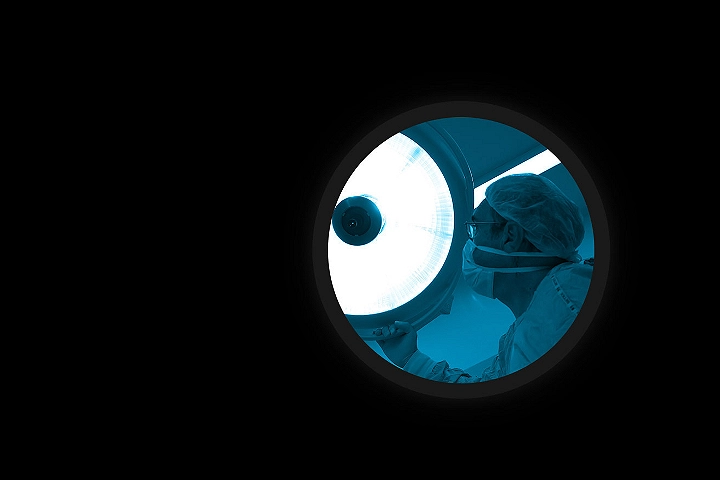
2023 Global Health Care Outlook
The pandemic that changed everything
COVID-19 has had a profound effect on how health care is being practiced in both industrialized and developing countries. It has changed global demands for an increased focus on sustainability and resiliency which was not present prior to the epidemic. What stands out most is that, after the pandemic, we will never be able to think about health care in the same way again. In our 2023 Global Health Care Outlook, we examine the current state of the sector and explore insights around international health policies, identifying emerging threats to public health, and how technology will change health care delivery over the next decade. We also look at the five key areas that are critical to this transformation, and we pose questions and suggest actions that professional can take to lead this transformation.
Explore and download the key issues below:
Virtual health delivery
The future of health care is here.
While COVID-19 demonstrated new ways that remote interactions can improve patient care and lower costs for providers, it has also raised new concerns about sustainability of current health care models. Virtual health delivery is not a substitute for traditional care, instead, it offers new ways of care delivery that were not possible in the past. It has the potential to inform, personalize, accelerate, and augment people’s ability to care for one another. The time has come to embrace emerging technologies and design health care delivery for the future. With over one billion people worldwide without any form of medical care and almost a billion people who have no access to modern medicines, virtual health will present an opportunity to change lives and make a difference.
Key takeaways:
- One of the first steps toward embracing virtual health is the adoption of electronic health records (EHR), which can provide a more comprehensive picture of population — as well as individual — health.
- As more digital health technology is incorporated into clinical processes through cloud computing, machine learning, and internet-connected devices, it can significantly reduce care costs. In addition, technology offers a solution to the shortage of critical care physicians.
- While mental health services were seen at the forefront of virtual health during the pandemic, they also are finding a growing following among mobile users. Apps are seen helping to manage mental health conditions such as anxiety or depression and help improve general well-being by encouraging behavior change.
Digital transformation
The rise of innovation in health care
As the world witnessed a sudden surge in the number of patients, increased health care demands, labor shortages, and supply chain issues during the pandemic – adoption of new technologies such as telemedicine and electronic health records (EHRs) proved to be the most efficient solution for providers to address these challenges. Digital technology attempt to reduce costs, deal more effectively with the changing patterns of demand, address a shrinking clinical workforce, and prepare better for the next global health crisis.
Key takeaways:
- COVID-19 accelerated the shift to cloud-based technologies designed to strengthen business operations and drive more customer interactions into the digital realm. This trend is forcing the large EHR providers to migrate their products and services to the cloud and develop partnerships with Customer Relationship Management (CRM) and Enterprise Resource Planning (ERP) providers.
- Emerging technologies such as AI, telehealth, blockchain, and monitoring devices, such as sensors, wearable and ingestibles, are providing real-time and continuous data about our health and our environment. This is redefining the future of health care and health delivery.
- Due to increased exposure to cloud technology, hospitals already are prime targets for ransomware attacks and other cybercrime. One way to prevent such attacks would be to apply blockchain technology to health data.

Health equity
Advance health equity as an outcome, not as an afterthought
The global health ecosystem observes great disparities based on age, location, gender, income, race, ethnicity, religion, and sexual orientation, despite significant efforts to eliminate them by health care providers, insurers, government agencies, aid organizations, and others. The COVID-19 pandemic further underscored the pervasiveness of health inequity. The virus disproportionally affected the most vulnerable groups, and focused public attention on how communities are only as strong as their most compromised members. As a result, many health organizations are rethinking how to address health inequity. For organizations, addressing biases and advancing health equity is not merely a moral imperative but also a competitive advantage. A coordinated effort among policy makers, industry executives, government officials, social influencers, and community organizers to close the widening global health equity gap.
Key takeaways:
- The social, economic, and environmental circumstances that together determine the quality of the health of the population, can have a greater impact on health outcomes than the care provided by clinicians.
- A key measure of health equity is life expectancy. If people living in the same geographical areas have significant differences in the life expectancies, it can spotlight the drivers of health inequities. The pandemic added to the health equity divide, affecting access to food, childcare, stable housing, and income.
- Racism and bias also threaten the adoption of new technologies that could provide better care delivery to these underserved populations. Telemedicine is a key component of the digital transformation of health care since the COVID-19 pandemic, but it hasn’t been adopted by all populations equally.

Sustainability
Making climate change a global priority
Climate change is a universal risk to human health and well-being. As these risks mount, providers face the challenge of maintaining the quality of care in the face of mounting financial pressure. What’s more, a changing climate requires greater disaster preparedness, especially in economically disadvantaged regions. While treating the health consequences of climate change falls to the global health care sector, they are also a contributor to the rising carbon levels driving climate change. Responding to these threats requires health systems that are more resilient and sustainable. But the challenge still remains. How are the leaders preparing themselves for a better future?
Key takeaways:
- Health organizations must be prepared to provide care in the wake of natural disasters, ensure the supply of medicine amid weather-related disease outbreaks, and adopt practices that reduce waste.
- While emissions remain one of the biggest challenges, health care facilities also are looking for ways to reduce waste and boost sustainability. More providers are adopting recycling and waste management programs, substituting single-use materials with reusable ones where practical and adopting local suppliers where possible to minimize supply disruptions.
- The pandemic added an urgency to make supply chains more sustainable. Therefore, care providers are looking for improvements in delivery methods, such as virtual care.

Workforce
Building a more sustainable workforce
The COVID-19 pandemic has exacerbated existing workforce challenges in health care and resulted in fundamental changes to how work gets done — who does what and where they do it may have changed permanently. In some ways, the global demographic shifts in health care that are occurring post-pandemic have always existed, but COVID-19 has compounded them. Organizations need new thinking about the workforce and how its structured. Continued investment, and an efficient use of capital, are essential to ensure the health industry continues to meet rising global demand. These new models will help to make health care more sustainable and effective for the workforce and produce better outcomes for patients.
Key takeaways:
- By 2030, the global health care sector will need an estimated 80 million more workers to meet demand, and about 18 million of those will be needed for low-income countries. Yet even as the demand for clinicians mounts, doctors and nurses increasingly say they plan to reduce their work hours.
- With the changing workplace demands, health care providers are creating more appealing and sustainable work environments by focusing on improving workplace culture and communications, as well as prioritizing mental health services for employees and patients alike.
- The skills shortage, combined with mounting margin pressure, has prompted many health organizations to turn to technology and new approaches — such as telemedicine and “hospitals from home”—to address the gap and drive greater cost efficiencies.